Hospitalisations of Aboriginal children too high
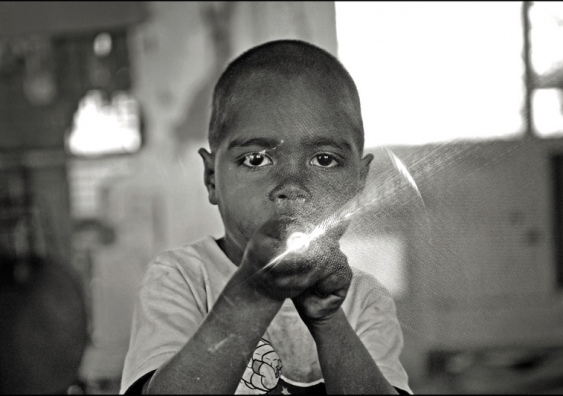
Avoidable hospitalisations among Aboriginal children are almost double those of non-Aboriginal children, UNSW research has revealed.
Avoidable hospitalisations among Aboriginal children are almost double those of non-Aboriginal children, UNSW research has revealed.
Dan Wheelahan
UNSW Media Office
02 9385 1933 or 0435 930 465
d.wheelahan@unsw.edu.au
UNSW research shows avoidable hospitalisations among Aboriginal children are almost double those of non-Aboriginal children.
The study, the first to investigate avoidable hospitalisations for common childhood conditions in Aboriginal and non-Aboriginal children, analysed NSW hospital admissions data for more than a million children born between 2000 and 2012. Researchers identified 365,000 avoidable hospitalisations among children during this period.
The study, published today in BMC Pediatrics, found Aboriginal infants were twice as likely as non-Aboriginal children to be hospitalised for conditions that could have been prevented or treated outside of a hospital.
Lead researcher Dr Kathleen Falster, a visiting Fellow with the Centre for Big Data Research in Health at UNSW, said more needs to be done to monitor and prevent avoidable hospitalisations in children, especially Aboriginal children.

Dr Kathleen Falster. Photo: supplied.
“There should be no difference in avoidable hospitalisations between Aboriginal and non-Aboriginal children,” said Dr Falster, who also works at ANU’s Research School of Population Health and the Sax Institute.
“The good news is that this study shows we can make a big difference to children’s lives, because these hospitalisations are largely preventable.”
This study also found a significant gap between Aboriginal and non-Aboriginal children in every part of NSW.
We also need to ramp up prevention efforts, such as quit smoking programs for new parents, because smoking has a big impact on respiratory illnesses in infants.
“It doesn’t matter if children live in a poor area or a wealthy area, in the city or remote communities, there is a big gap,” she said.
Dr Falster has called on governments to routinely monitor child-specific avoidable hospitalisations in Australian children.
“At the moment the measure used is mostly focused on adult diseases, so you aren’t going to pick up on the areas where you could improve things for children,” Dr Falster said.
“A child-specific measure, like the one we used for the first time in this study, could be incorporated into routine government reporting to support action to close the gap, and target efforts effectively.”
Chief Investigator and Aboriginal health research leader Professor Sandra Eades, from Baker IDI, said many of the health issues were easily preventable.
“We need to support and enhance affordable family-friendly health services, particular Aboriginal Community Controlled Health Services who are on the front line caring for families,” she said.
“We also need to ramp up prevention efforts, such as quit smoking programs for new parents, because smoking has a big impact on respiratory illnesses in infants.
“Many of the illnesses causing these hospitalisations have also been linked to overcrowded and poor quality housing. Policies that support affordable and quality housing for Aboriginal and disadvantaged families are also part of the solution.”