UNSW researchers lead Cancer Council funding round
The grants will help UNSW researchers who are engaged in promising work to overcome pancreatic, breast, bowel and childhood cancers.
The grants will help UNSW researchers who are engaged in promising work to overcome pancreatic, breast, bowel and childhood cancers.
Lucy Carroll
UNSW External Communications
9385 8732, 0402 005 319
l.carroll@unsw.edu.au
Researchers examining dual treatments for pancreatic cancer and overcoming endocrine resistance in breast cancer are among four projects to receive support in the latest round of funding from the Cancer Council NSW.
The projects are among 13 ground-breaking cancer research studies receiving a share in $9 million in grants that will announced at Cancer Council NSW’s annual Research Awards in Sydney tonight.
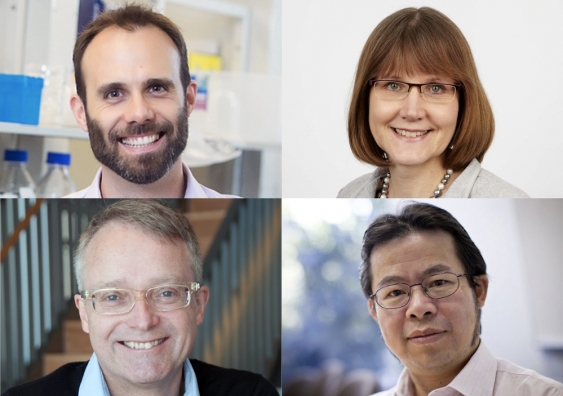
Dr Thomas Cox, from the Garvan Institute of Medical Research and conjoint senior lecturer at UNSW Medicine, has received $450,000 to try and boost the effectiveness of chemotherapy in pancreatic cancer by combining it with another treatment that blocks the production of connective tissue that can act to protect the tumour.
Pancreatic cancer tumours feature high levels of connective tissue which provide cancer cells with protection from chemotherapy and other treatments. Dr Cox’s team has recently discovered a drug which can stop the connective tissue from being produced and combined with standard chemotherapy could co-target pancreatic cancer.
In this project, the team will use 3D models, which mimic cancer progression and tissue growth, with state-of-the-art imaging to try and maximise effective treatment and minimise toxicity.
“This funding will be critical in supporting the early stage development of a potentially new and revolutionary approach to treating the devastating disease that is pancreatic cancer,” said Dr Cox. “It will mean we can establish a pre-clinical data portfolio to support the potential transition of this new approach into Australian clinical trials.
“My team is immensely grateful for the generosity and support of Australians who donate their hard-earned dollars to support research that would otherwise not be possible.”
Professor Christopher Ormandy, from the Garvan Institute of Medical Research and conjoint professor at UNSW Medicine, has received almost $450,000 to investigate targeting a protein (ELF5) as a new treatment to prevent hormone therapy resistance in patients with estrogen receptor positive breast cancer.
Two-thirds of breast cancers are estrogen receptor positive, which means cancer cells are dependent on estrogen to grow. After surgery, patients are often treated with hormone therapy to block the effects of estrogen. If there is a recurrence cancer cells can become resistant to hormone therapy.
“We hope to establish targeting ELF5 as a new therapeutic strategy to prevent or to delay resistance to hormonal therapy for breast cancer,” said Professor Ormandy. “If we are successful we will produce preclinical data supporting the trial of drugs targeting ELF5 action as a way of extending the utility of hormone therapy.”
Associate Professor Maija Kohonen-Corish, senior visiting fellow at St George & Sutherland Clinical School, has received $450,000 to build evidence on the alteration of a certain protein, called MCC (mutated in colorectal cancer), with the aim of creating new treatment targets and biomarkers for bowel cancer.
This research team has discovered that the lack of MCC causes a disruption in the function of other key proteins in the colon and this promotes the development of an invasive type of colorectal cancer.
Associate Professor Kohonen-Corish’s team will test possible therapies in MCC-altered bowel cancer by exploiting the tumour’s vulnerability caused by DNA damage. The team will explore the effectiveness of two drugs, irinotecan and PARP inhibitors. They will apply these drugs separately and in combination to cells that either have normal MCC or lack of it and compare the effects.
“After years of work, we are closing in on the key role of the MCC gene in cancer and will show how it could be exploited to improve cancer therapy,” said Associate Professor Kohonen-Corish.
Associate Professor Tao Liu, from the Children’s Cancer Institute, has received $450,000 to investigate a new targeted treatment for neuroblastoma, the most common solid tumour in early childhood.
Most people with advanced neuroblastoma die of the disease, and survivors suffer from life-long adverse effects due to high-dose chemotherapy which is the current standard treatment. One subtype with a particularly poor prognosis is neuroblastoma caused by rearrangements in a gene called TERT that result in uncontrolled cancer growth. Only 20% of children with this type of neuroblastoma survive.
Professor Liu said his team are investigating how particular proteins affect the development and growth of tumours in children with TERT-rearranged neuroblastoma. In this study, the team will examine the role of a protein called CDK7. They also aim to explore how best to target and inhibit the action of this protein to stop cancer cell growth.
Dr Jane Hobson, Research Grants Manager at Cancer Council NSW said: “We are extremely proud to announce another round of extraordinary projects in 2019. We are confident these projects will provide incredible value to cancer patients and continue to push our progress towards a cancer free future.”
Funds have been awarded to projects deemed through peer review to be of the highest scientific merit; and through consumer review to be of the most value to the community supporting Cancer Council.
“The broad range of projects that we fund – across many types of cancers and stages of the cancer journey – shows Cancer Council NSW’s commitment to work across every area of every cancer,” Dr Hobson said.