Last week the New South Wales government announced schools are scheduled to re-open in October. While face-to-face learning undoubtedly has benefits for both children and parents, the announcement left unanswered a series of important questions about how this can be done safely.
By the time NSW lifts restrictions (estimated to be around October), only 60-70% of the population in NSW — and possibly less in Australia — who are 16 years and over may be fully vaccinated.
The Australian Technical Advisory Group on Immunisation (ATAGI) has recommended vaccination for children 12 and over, but most of these children will not be fully vaccinated by October, and children under 12 will remain unvaccinated for now.
In NSW, with well over 1,000 cases a day and rising, there will still be substantial community transmission when schools open. It is unclear when schools in Victoria (where cases are also on the rise) will open, but there may still be some transmission in the state when they do.
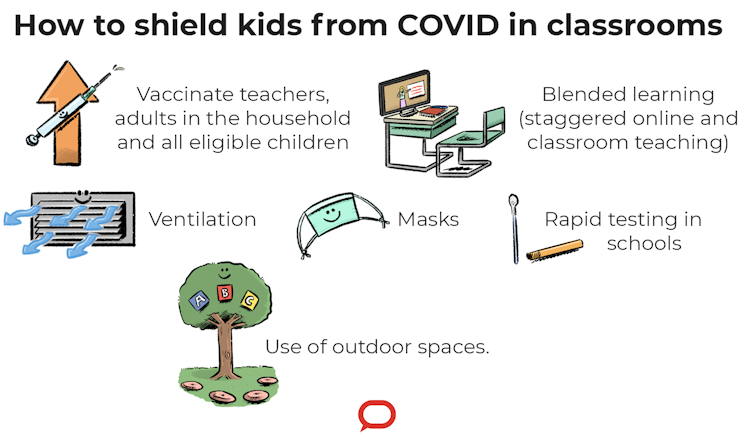
So, what do we need to do to make sure kids are as safe as possible at school?
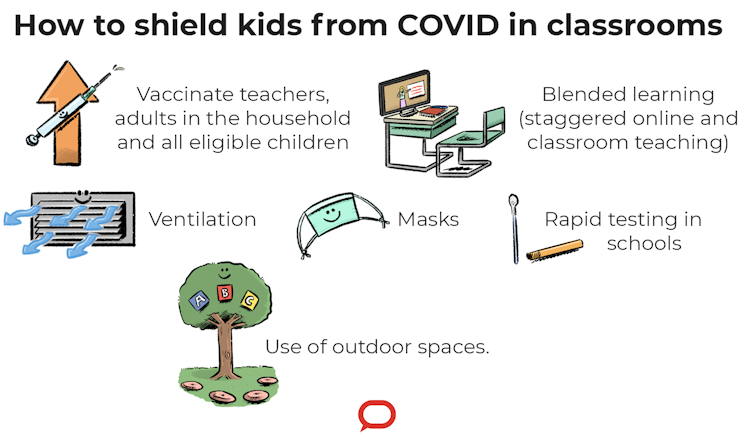
The Conversation, CC BY-ND
1. Vaccinate the adults around them
In California, a primary school outbreak occurred when an unvaccinated teacher, who came to work despite symptoms, read to students with their mask off. Most kids who became infected were well over 2 metres from the teacher, which confirms the 1-2m distancing rule is not effective for an airborne virus.
Every child and teacher in a classroom or childcare centre with an infected person is at risk. Shared air is the major way SARS-CoV-2 — the virus that causes COVID-19 — spreads.
Children often get the virus from the adults around them, so vaccinating adults in a child’s household, and teachers, can help protect them.
Vaccination is now mandatory for teachers in NSW, but around 67% have had one dose. This probably corresponds to less than 40% of the NSW population being fully vaccinated.

Anyone in the same room with an infected person, especially if that person isn’t wearing a mask, is at risk of catching the virus. Shutterstock
One dose of vaccination gives about 31% protection and two doses gives 67% (AstraZeneca) to 88% (Pfizer) protection against the Delta variant. Most kids will still be unvaccinated if schools in the two largest states re-open for the last term of the year. This means it’s even more important to ensure the adults are vaccinated.
2. Mandate masks for teachers and students
We can mandate masks in schools for teachers and students, and highly recommend mask use for younger children in childcare.
The American Academy of Pediatrics recommends masks for children two years and up; children over this age can wear masks without much trouble.
As mask use in schools has been more common overseas, there are now numerous toolkits (including translated versions) and recommendations to support children to wear a mask. For example, your child is more likely wear a mask if it has their favourite colour, sports team, character or special interest on it.
Importantly, a DIY cloth mask can be made to fit your child’s face and be high quality if key design principles are followed. It is important to ensure children have choices and understand the reason why they are wearing a mask (for instance: “When we wear a mask, the virus can’t jump from person to person.”
3. Ventilated classrooms
Classrooms can be ventilated by opening windows (ideally two windows at opposite ends of the room). If there is only one window, a fan can help move the dirty air out. If opening windows is not possible there is fortunately a cheap fix available — portable air purifiers, which dramatically reduce the viral load in classrooms.
There are DIY methods for making air purifiers, too.
4. Reduce numbers of people indoors
Reducing the number of people packed together in a classroom can reduce the risk of COVID. For example, during high epidemic periods, if the decision is made to open schools, a group of kids can come in every second day and learn online on alternate days.
We have shown this approach, when combined with masks, reduces the risk of transmission on university campus.
Use of outdoor spaces for lessons is also a smart move as the weather gets warmer. While Delta can transmit outdoors, the risk is likely much lower.
5. Test school kids
Finally, rapid point-of-care testing in schools will help reduce transmission, and self-testing kits (when approved in Australia) can help.
Saliva tests are also a practical way to test children. These tests are now available in official health settings, so governments could make them available to schools.
What about childcare centres?
We also need to consider childcare centres. Contrary to popular narrative, a new study shows kids up to three years old transmit more than older kids. So, vaccinating childcare workers and parents of young kids is also essential.
All the measures above, except masks for 0-2 year olds, can easily be used in childcare settings.

Rapid testing in schools could help reduce transmission. Shutterstock
Record numbers of children are being hospitalised with COVID-19 in the USA. It remains unclear whether the high numbers of sick children are due mostly to Delta’s increased transmissibility, or whether it also causes more severe disease in children, as it does in adults. Although the risk of severe disease remains much lower in children than adults.
One thing we do know is that as vaccination rates increase in adults, unvaccinated groups, the largest of which is children, will be proportionally more at risk. The 70-80% targets for vaccination of eligible adults for relaxing restrictions corresponds to 56-64% of the whole population, which leaves plenty of room for Delta to spread like wildfire in unvaccinated adults and kids. So there is good reason to protect kids if we open schools.
In addition, the productivity losses from lockdowns are an important component of the estimated A$220 million daily economic cost in NSW alone. Sick kids make it harder for their parents to work productively, if at all. And they make it more likely parents themselves become sick and are unable to work.

C Raina MacIntyre, Professor of Global Biosecurity, NHMRC Principal Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW; Greg Kelly, Senior lecturer, The University of Queensland; Holly Seale, Associate professor, UNSW, and Richard Holden, Professor of Economics, UNSW
This article is republished from The Conversation under a Creative Commons license. Read the original article.