First baby born in Australia through new fertility treatment developed by UNSW researchers
The CAPA-IVM treatment involves fewer hormone injections than traditional IVF, at a significantly lower cost.
The CAPA-IVM treatment involves fewer hormone injections than traditional IVF, at a significantly lower cost.

Sarah Forster
0408445694
sarah.forster@inthemediapr.com.au
UNSW Sydney and the Royal Hospital for Women are celebrating an Australian first, following the arrival of a baby conceived via a new clinical procedure to treat infertility.
After Leanna and Theo Loutas struggled for two years to fall pregnant, trying various treatments methods including a round of in-vitro fertilisation (IVF), Leanna was offered CAPA-IVM (Capacitation in-vitro maturation). This new treatment involves retrieving eggs at an immature stage and bringing them to maturity in cell culture, eliminating the need for the patient to undergo two weeks of hormone injections.
It was the research of Professor Robert Gilchrist from UNSW Medicine & Health, in partnership with researchers from Brussels and Saigon, that led to the development of CAPA-IVM.
“Many years of blood, sweat and tears have gone into this. Countless hours of research over two decades, so this is a very proud moment,” Prof. Gilchrist says.
“To be able to take a discovery from the lab into a clinic and make a real difference for Leanna on her fertility journey and other women who will follow is very special."
Read more: New IVM fertility treatment available for Australian women
Professor Bill Ledger from UNSW Medicine & Health, who is The Royal’s head of Obstetrics and Gynaecology, says that baby Bonnie’s arrival is particularly special.
“We’ve all been looking forward to seeing this baby come into the world. The Royal Hospital for Women is one of only six locations in the world to offer CAPA-IVM and this is the first baby conceived here in Australia through this method,” Prof. Ledger says.
“While this is a special time for Leanna and Theo as they enter the journey of parenthood, it’s a big moment for everyone involved, as we close the loop from research to the arrival of a baby."
While standard IVM has been a treatment option for many years outside Australia, and currently in Perth, CAPA-IVM is considered a step forward because it uses a new technique and pregnancy rates per cycle are higher.
“The problem has been when you take an egg out of the human body it matures very quickly, even when it may not be ready to, but the CAPA method switches off the progression of the egg for 24 hours. So it grows more slowly, and it matures more healthily,” Prof. Ledger says.
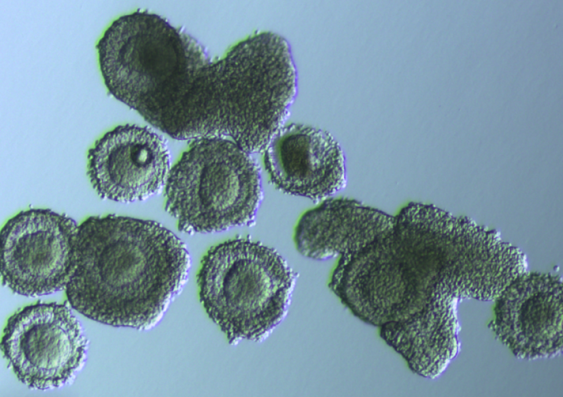
The CAPA-IVM fertility treatment involves retrieving eggs at an immature stage and bringing them to maturity in cell culture. Photo: Supplied.
According to Prof. Gilchrist, being able to take an egg out of the ovary before it has reached maturity makes the process a lot easier on patients.
“The principal advantage of CAPA-IVM is that it uses only two days of hormone treatment compared to two weeks of hormone treatment in an IVF cycle. So the burden is much less on the patient,” Prof. Gilchrist says.
“We’ve got quite a special treatment here because these women have only two days of hormones and have a reasonable prospect of getting pregnant.”
Read more: One in three women have a baby in their first IVF cycle: report
For Leanna, CAPA-IVM meant that she was able to travel and celebrate Christmas, without the stress of fitting in two weeks of hormone injections.
“I was going to take a break before trying IVF again as I didn’t want all of the side effects of the hormones while traveling. When I was offered CAPA IVM, I was pleasantly surprised to learn that I would only need to do two days of injections. It made the whole process seem a lot less daunting,” Leanna says.
“The treatment was a success and we were able to freeze two embryos. It was the best Christmas present we could have possibly had. We feel hugely privileged and grateful to have been given this opportunity. Hopefully we’re the first of many to come and when other people hear about our story it will give them encouragement.”
Find out more about CAPA-IVM through the Fertility and Research Centre at The Royal Hospital for Women.